Work-N-Progress ~ Last saved Oct 11, 2021 @ 1:02 pm
If you are a politically-active midwife trying to figure out how the formal practice standards for Ca LM became such a blankety-blank mess, this series will provide you with the historic background and more facts and information than you ever wanted to know.
But if you are in a big hurry, you can save this Intro at a later time and just go on to #1.
Midwifery ~ the World’s First and Oldest (5,00o & counting!) healthcare profession
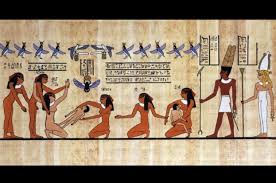 Five thousand year-old Egyptian hieroglyphics have memorialized midwifery as the first and the oldest form of organized healthcare service. The lives and practices of midwives are record in many places in the Judeo-Christian Bible.
Five thousand year-old Egyptian hieroglyphics have memorialized midwifery as the first and the oldest form of organized healthcare service. The lives and practices of midwives are record in many places in the Judeo-Christian Bible.
Historically and factually, midwifery is a primary women’s profession. While reading an article about gender roles, the author mentioned that in 1930, US Census had only occupational category was 100% female and that was midwifery. So far the 400-plus California midwives licensed by the Medical Board are all female. As a women’s occupation, we often find ourselves on both ends of this equation — at one time being pregnant or the laboring woman being cared for by our midwives (or L&D nurses!), and on another occasion being the midwife who is providing care to another childbearing woman.
 We learn about pregnancy and childbearing from inside our own bodies, as a series of direct experiences. This not only includes biological sensations but also the psychological aspects of childbearing, such as its ‘normal’ anxieties, emotional ups and downs and the extraordinary feeling when we push our baby out under our own power!
We learn about pregnancy and childbearing from inside our own bodies, as a series of direct experiences. This not only includes biological sensations but also the psychological aspects of childbearing, such as its ‘normal’ anxieties, emotional ups and downs and the extraordinary feeling when we push our baby out under our own power!
Normal childbirth is biologically and sociologically a woman-centered activity for mothers and midwives both

As students of midwifery, women are intimately familiar with their own gender-related biological functions. Even if a midwife has not given birth herself, she still has personal experiences with the female physiological of reproduction and sexuality.
Biologically and hormonally, the spontaneous onset and progression of labor, birth and breastfeeding are all aspect of normal female sexuality — same physical body parts, same realm of biological activity, and same endocrine system. In relation to sex, childbirth and let-down of breast milk, women have two opposing sets of hormones: oxytocin & beta endorphins to fuel normal biological progresses and adrenaline and cortisol to put the brakes on them if its not safe to have sex or woman perceives the situation as unsafe for herself or unborn baby.
One can imagine a cave-dwelling pregnant woman in early active labor meandering around the near-by woods surrounding their campsite when she suddenly hears a grizzly bear crash through the trees. As she spots his huge black bulk coming in her direction, a powerful surge of adrenalin instantly stops her labor, while dramatically increasing her heart and respiratory rate, fueling her thigh muscles and laser-focusing her brain to better see her surrounding so she can swiftly race back to safety.
However, it will take several hours to metabolize all the adrenaline and cortisol, so it may be 5, 10 or even 20 hrs before spontaneous labor begins again. Then oxytocin and beta-endorphin hormones will one again trigger the physiological processes resulting in cervical dilatation and expulsive uterine contractions that will push the baby out into the safety of their cave home and protection of family members and familiar women helpers.
It must be noted that many of our physiological processes are a blend of biology and psychology. As an ER nurse, this was regularly demonstrated when trying to collect a urine sample. As long as I was standing by the bedside watching, my patient would be unable to “pee the a cup”. What did work was telling the patient that i would leave them alone for several minutes and then pull the curtain snuggly around the bed to assure the patient’s privacy.
This direct relationship between biology, psychology, and at times sociology, applies to sexual arousal, our appetite and desire to eat (if scared, very worried or upset people either refuse food or throw-up their last meal). We often can’t fall asleep if worried or agitated and find ourselves holding our breath or hyperventilating when afraid. We even can get so terrified that we pass out cold.
Sexual function and spontaneously progressing labors both require that the natural process not be disturbed. Naturally progressing sexuality and childbirth both require personal privacy, confidence that you will not be interrupted and control over one’s environment that provides a quiet and soft of low lights. This is the polar opposite of the traditional hospital scene when the mother is put in stirrups and the overhead OR light is aimed at her crotch while as many as 11 hospital staff members stand around the bed with eyes glued to the mother’s perineum.
When discussing this in childbirth education classes or for my clients, i use the example of having (actually not having!) sex, or being very verbally constrained when one’s in-laws are visiting and sleeping in the next bedroom.
As a result, we know from direct experience what works and what doesn’t. For many of us, our first childbirth experience was an unnecessarily interventive hospital birth. We know all too well what it’s like to be a “labor patient” that is told to lie down, shut up and hold still so the “doctor can deliver your baby”.
As a result, the safety and well-being of childbearing women and the personal and professional interests of practicing midwives are naturally and intimately intertwined. From the standpoint of midwifery training and its legally-regulated practice, mothers and midwives are both served by midwifery’s protective and normalizing philosophy, its time-tested principles and worldwide guidelines for safely supporting pregnancy and childbirth in essentially healthy women with normal pregnancies.
Preparation and training for the practice of midwifery dramatically different than other forms of health- and medical care
The educational process for non-maternity care professions and allopathic medical education of MDs is startlingly different than that for most traditional (i.e. direct-entry, non-nurse) midwives. Future cardiologists don’t prepare for their role as a heart specialist by having a heart attack and then trying to nurse themselves back to health. Residents in a surgical program don’t begin by taking out their own appendix; neuro surgeons don’t practice by first operating on their own brain.
Future doctors acquire their knowledge indirectly by observing patients. No many how many times they stand by and observe a mother-to-be in labor or while giving birth, the medical student doesn’t have any direct biological experience, no physical sensations, none of the natural anxiety associated with months of pregnancy, the natural fear associated with the pain of childbirth and the worry that you or your baby might have a “bad outcome”.
 Historically, this was not true for midwives. According the demographic research spanning several centuries and many different countries, the “average” midwife begins by apprenticing with an older experience midwife when the apprentice’s youngest child was at least 10 or more years old. The average length of an apprenticeship was about 10 years, so most of women did not begin practicing independently until they were in their forties or even older.
Historically, this was not true for midwives. According the demographic research spanning several centuries and many different countries, the “average” midwife begins by apprenticing with an older experience midwife when the apprentice’s youngest child was at least 10 or more years old. The average length of an apprenticeship was about 10 years, so most of women did not begin practicing independently until they were in their forties or even older.
The historical art of midwifery is an interpersonal-relationship of trust between the mother and her midwives. Each licensed midwife should uphold the dignity and honor of the profession and accept its self-imposed discipline, which includes a responsibility to uphold professional standards, avoid compromise based on personal or institutional expediency, and adhere to professional rather than commercial standards in making known the availability of their services.
On a practical level those services must be predicated on modern biological science of childbearing. Obviously that changes and evolves with time, so the education of a practicing midwife is lifelong process.
If asked to defined the objective of midwifery as a profession in a single sentence, I would say that it is to render our services to childbearing women and their infants with full respect for human dignity. This balances principles of modern medical science with the right of an individual healthy childbearing to decline interventions that she believes are not in her best interest.
{♥link to ACOG’s Ethical Committee Opinions # 166 and # 214♠}
Women labor to bring forth life. We know that giving birth is not easy. Our creativity, our fecundity needs time, space and nourment in order to come to fruition. Sometimes poems are born, sometimes visual images or new ideas, sometimes the next generation. We affirm life with our love. We love with intensity, and gentleness. We bear the pain of seeing such that we love die unnatural deaths — from wards, ecological disaster, indifference. We continue to love Our strength is sustaining.
You must log in to post a comment. Log in now.