Updated ~ Jan 22, 2021
Easy-to-share Tiny URL:
https://tinyurl.com/y2w57axc {y2w 57 axc}
Jan 14, 2021
 Medical Board of California
Medical Board of California
Interested Parties Meeting on the
Standard of Care for California Licensed Midwives (SCCLM)
by Faith Gibson, LM
Information for attendees of the Interested Parties meeting on the Standard of Care for California LMs (SCCLM) adopted by the MBC in 2005 (per SB 1950) and post-AB 1308 Practice Guidelines uploaded to the Medical Board’s web site in May of 2014.
Into and Overview
NOTE: I am the author and editor of the original version of the Standard of Care for California Licensed Midwives (SCCLM) authorized by SB 1950.
Prior to passage of AB 1308, the SCCLM was the legally authorized standard of care from 2006 to 2013. However in 2013, AB 1308 repealed the SCCLM in its entirety. In May 2014, the Medical Board posted a drastically changed version of the previous SCLLM that was titled Practice Guideline that had not been approved by the Office of Administrative Law (OAL), thus the two documents are not interchangeable and the legal authority of the 2006 SCCLM does not apply to the MBC’s Practice Guidelines
In discussing the topic of midwifery standards for licensed midwives and the MBC’s version of Practice Guidelines posted in 2014, I must emphasis a critical difference between the two documents in addition to their respective legal status.
The SCCLM is a highly integrated document approved by the OAL that is legally required to be taken as a whole, as its principles and provisions are a single unit that requires information in other parts of the document to interpret any individual policy, principle, or practice.
Without having the full text of the document as reference, there is no way to know if the reader is missing critical information when interpreting a specific provision.
Drastic changes in women’s reproductive right due AB 1308
Unfortunately, AB 1308 deleted or drastically changed the most fundamental aspect of the California Licensed Midwife’s standard of care. For the profession of midwifery, the woman’s right to self-determination is the “First Principle” and core of our professional standard of practice. However, all provisions that identified and acknowledged the childbearing woman’s “moral right to bodily integrity” and “respect for the patient as a person” [see ref. #1 below] were not included when the Board deleted the SCLLM and replaced it with its 2014 Practice Guidelines based on AB 1308.
This First Principle is not an idea made up by California licensed midwives, as respect for a childbearing woman’s right to self-determination it is true the world over.
It is incorporated into midwifery Standards and Codes of Ethics by professional midwives in other states, in the policies of the Midwives Alliance of North America (MANA – US & Canada), College of Midwives of British Columbia’s Standards of Practice and the International Confederation of Midwives (ICM) and to the great surprise of nearly everyone, the published policies of the American College of Obstetricians and Gynecologists.
ACOG Committee Opinions on Reproductive Rights of Women
ACOG’s Committee Opinions #166 — Informed Refusal, 1995 & #214 — Patient Autonomy: The Maternal-Fetal Relationship“, 1999 were published in ACOG’s 2000 Compendium (pgs 134 & 160).
These policy opinions, among many other similarly supportive statements, say that:
- Abiding by the patient’s autonomous decision will provide the best care for the pregnant woman and the fetus in most circumstances.
- In the event of an emergency … the obstetrician must respect the patient’s autonomy, continue to care for the pregnant woman, and not intervene against the patient’s wishes regardless of the consequences.
- When a patient’s autonomy is violated, the woman is wronged and may be harmed, whether physically, psychologically or spiritually.
- The patient’s subsequent loss of trust in the healthcare systemmay reduce the health care provider’s ability to help her and may deter others from seeking care.
ACOG’s Statement of Policy #1067 on Abortion says, among other supportive statements:
- The diversity of beliefs should be respected
- Informed consent is an expression of respect for the patient as a person; it particularly respects a patient’s moral right to bodily integrity, to self-determination regarding sexuality and reproductive capacities and to the support of the patient’s freedom with caring relationships
- The pregnant women should be fully informed in a balanced manner about all options … the professional should make every effort to avoid introducing personal bias
Section V of the SCCLM modeled after ACOG Opinions #108, #166 & #214
As author and editor of the SCCLM, I used ACOG Committee Opinions #108, #166 and #214 definition of patient autonomy and a woman’s ethical right to self-determination as the model for provisions in the SCLLM acknowledging the ethical rights of clients who are being cared for by licensed midwives. I also used the very similar but midwifery-specific language in the College of Midwives of British Columbia’s Standards of Practice.
As ACOG’s statement applies to normal childbirth services as provided by obstetricians and licensed midwives, then ACOG and the SCCLM are in total and 100% agreement.
EDITOR’S NOTE: Source material for ACOG’s Committee opinion #108, #166 and #214 can be found in ACOG Committee Opinion #108, 1992 Ethical Dimensions of Informed Consent [ref #1]
Negative Impact of AB 1308
In light of ACOG own published opinions and policies that acknowledged informed consent as a “moral right to bodily integrity” and “respect for the patient as a person”, the drastic changes required by AB 1308 was shocking, inexplicable and unacceptable to California midwives and childbearing women.
AB 1308 specifically and only suspends the legal rights of childbearing women who are clients of licensed midwives or seeking care from a licensed midwife. It is not lost on licensed midwives that the rights that ACOG proudly stands by in its own published policies for labor patients and women seeking abortion services are the very same women’s reproductive rights that they eliminated when crafting the language for AB 1308.
What if these provisions in AB 1308 were applied to obstetrical providers of abortion?
What if mandatory evaluation of risk-factors was view from the other side of the fence? For example, what if Californians who do not support the State’s liberal abortion statutes cited, among other objections, the significant risk-factors associated with abortion to the mental, physical and future reproductive health of the woman?
What if this politically influential group lobbied the State Legislature to pass a bill requiring obstetricians who provided abortion services to first have their patients evaluated by a clinical psychologist, or if the pregnant woman belonged to an organized religious, a clergy member of her faith?
Under this legislative scheme, obstetricians would only be allowed to provide care if the evaluating psychologist, priest, minister or rabbi was willing to state that the “procedure“ was “not likely to affect” the “mental, physical and future reproductive health of the woman”.
ACOG doesn’t get to have its cake and eat it too
If essentially healthy pregnant women do indeed have the constitutional rights elucidated in its Committee Opinions #108, #166, #214 and #1067, then any insistence by ACOG that women who seek or receive midwifery care, out of all the childbearing women in the State of California, do NOT enjoy the same reproductive rights that ACOG so plainly acknowledges in its Opinions #108, #166, #214 and #1067 .
This dubious conclusion is not only illogical and irrational, but doubly discriminatory, as it discriminates against this class of childbearing women and discriminates against all California licensed midwives.
End of revision added Jan 22, 2010 @ 12:01 pm
Point-by-point review of the drastic changes introduced by AB 1308
“Before and after” comparisons of the specific text involved:
Prior AB 1308, the original version of STANDARD SIX read:
STANDARD SIX ~ The Midwife shall confer and collaborate with other healthcare professionals, including other midwives, as is necessary to professionally meet the client’s needs. When the client’s condition or needs exceed the Midwife’s scope of practice or personal practice guidelines, the Midwife shall consult with and refer to a physician or other appropriate healthcare provider.
After passage of AB 1308, the language in STANDARD SIX was deleted and replaced with this statement:
STANDARD SIX: The licensed midwife refers the client to a physician, as required by law, if at any point during a pregnancy, childbirth, or postpartum care the client’s condition deviates from normal.
The original SCCLM version of Section V read:
(a) Responsibility of the Licensed Midwife
With respect to the care of a client with a significant risk factor as identified by the client selection criteria in section IV, or other science-based parameters, the licensed midwife shall inform the client about the known material risks and benefits of continuing with midwifery care relative to the identified risk factor and shall recommend to the client that her situation be evaluated by a medical practitioner, and if appropriate, transfer her primary care to a licensed physician who has current training and practice in obstetrics.
(B) Client’s Rights to Self-Determination
In recognition of the client’s right to refuse that recommendation, as well as other risk- reduction measures and medical procedures, the client may, after having been fully informed about the nature of the risk and specific risk-reduction measures available, make a written informed refusal.
If the licensed midwife appropriately documents the informed refusal in the client’s midwifery records, the licensed midwife may continue to provide midwifery care to the client consistent with evidence-based care as identified in this document and the scientific literature.
The post-AB 1308 version for Section V struck these words from paragraph (a) — Responsibility of the Licensed Midwife
….shall inform the client about the known material risks and benefits of continuing with midwifery care relative to the identified risk factor and shall recommend medical practitioner and if appropriate, to transfer her primary care to a physician with training in obstetrics
When AB 1308 replaced the word “recommend” with “require”, it functionally gutted the both the ethical rights of childbearing women to make medical decisions for themselves and at the same time, it gutted the midwife’s professional duties to consult and collaborate with various other healthcare professionals who by training or experience are more knowledgeable about the situation than she. This includes more experienced midwives, family practice physicians with obstetrical privileges, obstetricians and other medical specialities.
Under the SCCLM, that full range of options included telephone consultations to collaborating with specialists (including obstetricians) to recommending, or in certain instances, requiring, a medical evaluation by a physician whose expertise is specific to the risk-factor in question. That may be an obstetrician, but when the issue concerns bodily organs or system not associated with the female reproduction, it may be an perinatologist, endocrinologist, hematologist or even a geneticist.
The response by the licensed midwife was, and should remain, determined by the nature of the “identified risk” itself. The ultimate goal it to consult, collaborate or refer the childbearing woman to a practitioner more knowledgeable in the client’s identified risk factor than than the midwife.
Unfortunately, those logical options for both mothers and midwives were all swept away by passage of AB 1308,
Section V in the 2014 Practice Guidelines now says:
Responsibilities of the Midwife
With respect to the care of a client who deviates from a normal pregnancy as identified by the client selection criteria in section IV or other science-based parameters, the licensed midwife informs the client that her situation must be evaluated by a licensed physician who has current training and practice in obstetrics and gynecology.
If the physician determines that the client’s condition or concern has been resolved such that the risk factors presented by a woman’s disease or condition are not likely to significantly affect the course of pregnancy, the licensed midwife can continue to provide primary care.
The client should further be informed that unresolved significant risk factors will limit the scope of the midwife’s care to concurrent care with a physician, regardless of whether the woman has consented to care or refused care by a physician.
It is recognized that the client has the right to refuse the recommended referral; however, pursuant to the law, the licensed midwife cannot continue care. The licensed midwife will document refusal of the referral in the client’s record.
Client’s Right of Self-determination ~ paragraph B — were entirely DELETED
In recognition of the client’s right to refuse that recommendation, as well as other risk- reduction measures and medical procedures, the client may, after having been fully informed about the nature of the risk and specific risk-reduction measures available, make a written informed refusal.
If the licensed midwife appropriately documents the informed refusal in the client’s midwifery records, the licensed midwife may continue to provide midwifery care to the client consistent with evidence-based care as identified in this document and the scientific literature.
My Conclusions:
When divorced from the provisions in the SCCLM, the Practice Guidelines as published on the MBC’s website in May 2014 are no longer internally-consistent or legally relevant. As a result of these omissions, deletions, and changes, concepts in the Guidelines have been misunderstood and misused by persons who did not appreciate the critical distinction between the original SCLLM and the MBC’s version of Practice Guidelines or the important legal distinction between the words recommend and require, which was either overlooked or disregarded.
As a result, the history, principles and provisions of the SCCLM of 2005 remain as relevant as the unofficial (not approved by OAL) Practice Guidelines of May 2014.
For that reason, I posted this information for attendees of the Medical Board’s Interested Parties Meeting held January 14, 2012

However, this overview would not be complete without these three truisms and a heartfelt request on behalf of mothers and midwives:
- The obstetrical and midwifery profession are in total agreement in our goal of making childbirth as safe as possible for every new mother and newborn baby in America.
- The midwifery profession acknowledges its duty to childbearing women to guard the public reputation of the obstetrical profession and obstetrical departments of hospitals so that women who need these services will say yes” instead of “no” when told that they would best be served by being hospitalialized and trusting the process of obstetrical care they receive from the nurses and physicians caring for them and their unborn babies.
- Someday in the 2st century the American obstetrical profession will extend the same professional respect for midwives that they expect from midwives.
California licensed midwives provide community-based care to an essentially healthy population of childbearing women, while obstetricians are required to provide critical care to women with high-risk pregnancies.
 Obviously we have very different experiences of our respective professions, but around the world childbirth is the very safest when midwives are a normal part of the mainstream healthcare system, women receive maternity care during pregnancy and physiological management of childbirth is the evidence-based standard of care for healthy women with normal pregnancies, and midwives and obstetricians have a mutually cooperative and respectful relationship with each other.
Obviously we have very different experiences of our respective professions, but around the world childbirth is the very safest when midwives are a normal part of the mainstream healthcare system, women receive maternity care during pregnancy and physiological management of childbirth is the evidence-based standard of care for healthy women with normal pregnancies, and midwives and obstetricians have a mutually cooperative and respectful relationship with each other.
Topics in this document
 The 2006 Standard of Care of California Licensed Midwives, the 2014 Practice Guidelines, ACOG Committee Opinions #108, 166 & 214, informed consent, legal issues associated with risk-reduction measures, AB 1308, the difference between the words “recommend” and “require“, the iatrogenic issue of Never Events, the history and legal status of midwifery in California, presidential Executive Order 9066 (Japanese Internment), the 1976 California Supreme Court Bowland Decision, midwifery licensing legislation for non-nurse midwives in 1917, 1949, and 1993, and useful background information on Senator Killea, author of the Licensed Midwifery Practice Act of 1993
The 2006 Standard of Care of California Licensed Midwives, the 2014 Practice Guidelines, ACOG Committee Opinions #108, 166 & 214, informed consent, legal issues associated with risk-reduction measures, AB 1308, the difference between the words “recommend” and “require“, the iatrogenic issue of Never Events, the history and legal status of midwifery in California, presidential Executive Order 9066 (Japanese Internment), the 1976 California Supreme Court Bowland Decision, midwifery licensing legislation for non-nurse midwives in 1917, 1949, and 1993, and useful background information on Senator Killea, author of the Licensed Midwifery Practice Act of 1993
Index
Part One: The Standard of Care of California Licensed Midwives (SCCLM)
Part Two: “Never Events” ~ When Health Care Harms in the Context of AB 1308
Part Three: History of Midwifery Legislation in California beginning

California Licensed Midwife Alison Price
Part One:
The Standard of Care of California Licensed Midwives (SCCLM)
The title page of the Purpose, Definitions & General Provisions of the SCCLM identifies the origin of its standards as consistent with those of other states, as well as national and international midwifery organizations:
I. This document provides a framework to identify the professional responsibilities of licensed midwives and permit an individual midwife’s practice to be rationally evaluated, to ensure that it is safe, ethical and consistent with the professional practice of licensed midwifery in California.
However, this standard of care document is not intended to replace the clinical judgment of the licensed midwife.
Sources and documentation used to define and judge professional practice include but are not limited to the following:
-
-
- The international definition of a ‘midwife’ and the midwifery scope of practice by the International Confederation of Midwives (ICM) & College of Midwives of British Columbia
- Customary definitions of the midwifery model of care by state and national midwifery organizations, including the Licensed Midwifery Practice Act of 1993 and all its amendments
- Standards of practice for community midwives as published by state and national midwifery organizations
- Philosophy of care, code of ethics, and informed consent policies as published by state and national midwifery organizations
- Educational competencies published by state and national direct-entry midwifery organizations
 Risk Factors, Risk-Reduction Measures, Informed Consent, the Midwife’s Responsibilities and Client’s Rights
Risk Factors, Risk-Reduction Measures, Informed Consent, the Midwife’s Responsibilities and Client’s Rights
California licensed midwives have an ethical and legal obligation to be knowledgeable about of known risks and to clearly communicate this information to prospective and current clients whenever a risk is identified and to document in the client’s chart that this disclosure was made. This is clearly spelled out in the original “Standard of Care for California Licensed Midwives” (SCCLM) adopted by the Medical Board in 2005 and approved by the OAL March 2006.
The ethical foundation of midwifery as a profession are the attributes of competency — midwifery education, clinical training — and the practitioner’s ability to identify biological and psychological conditions and social circumstances that may represent a risk to the childbearing woman and/or her unborn or newborn baby and take appropriate action.
Sections 4 and 5 (pages 4-7) of the SCCLM approved by the OAL in March of 2006 includes several provisions establishing the standard for community-based (ie. non-medical) mfry to acknowledge the childbearing woman’s constitutional rights of autonomy and self-determination and the midwife’s responsibility to respect them.
It must be noted that the right of clients to decline the midwife’s recommendation is an entirely different matter than refusing treatment for a current complication as required by the LMPA of 1993. No one – not midwives nor childbearing families — is arguing for the so-called “right” of pregnant women to go into convulsions from untreated pre-eclampsia or similar situations.
Provision III, entitled “STANDARD OF PRACTICE FOR COMMUNITY-BASED MIDWIFERY”, which starts on page 4 includes the following statements:
Standard Four: The midwife shall respect the autonomy of the mentally competent adult woman by working in partnership with her and recognizing individual and shared responsibilities. The midwife recognizes a healthy woman as the primary decision-maker throughout the childbearing experience.
Standard Five: The midwife upholds the clients right to make informed choices about the manner and circumstances of normal pregnancy and childbirth and facilitate this process by providing complete, relevant, and objective information in a non-authoritarian and supportive manner while continuously assessing safety considerations and risks to the client and informing her of same.
Standard Six: Midwife shall confer and collaborate with other healthcare professionals as is necessary to professionally meet the client’s needs. When the client’s condition exceeds the midwife’s scope of practice or personal practice guidelines, the midwife shall consult with and refer to a physician or other appropriate healthcare provider.
Section V is titled: “Risk factors identified during the initial interview or arising during the course of care”. It includes these two statements:
Responsibility of the Licensed Midwife
With respect to the care of a client with a significant risk factor as identified by the client selection criteria in section IV or other science-based parameters, the licensed midwife shall inform the client about the known material risks and benefits of continuing with midwifery care relative to the identified risk factor and shall recommend to the client that her situation be evaluated by a medical practitioner, and if appropriate to transfer her primary care to a licensed physician who has current training and practice in obstetrics.
Client’s Rights to Self-Determination
In recognition of the client’s right to refuse [the midwife’s] recommendation as well as other risk-reduction measures and medical procedures, the client may, after having been fully informed about the nature of the risk and specific risk-reduction measures available, make a written informed refusal.
If the licensed midwife appropriately documents the informed refusal in the client’s midwifery records, the licensed midwife may continue to provide midwifery care to the client consistent with evidence-based care as identified in this document and the scientific literature.
Recommending a consult is something that occurs frequency in all healthcare disciples as practitioners encounter situations, signs, or symptom about which they are not sure of the relevancy – maybe it signals a problem, maybe not. To be sure which is which, the streetwise practitioner recommends that the patient “consult with a “specialist” just in case.
This provision of the SCCLM is consistent with the usual and customary due diligence for healthcare practitioners of all disciplines requires that they recommend a “second opinion” from another professional who has additional training or expertise in the matter at hand – i.e. to consult with a specialist. However, this does not require that clients or patients take that advice.
In relation to midwifery, this would be a consultation or evaluation with an obstetrician, internist or endocrinologist, hematologist, etc. or whatever specialist is most appropriate to the pregnant woman’s potential risk factor or problem. All medical professionals and their lobbyists recognize this “usual and customary” practice for what it is – CYA.
Patients may or may not follow these recommendations, which are voluntary, as healthcare providers cannot legally force or coerce patients to have unwanted, or what they believe are unnecessary, medical evaluations or tests, even though most practitioners believe that all reducible risks should be reduced as much as possible i.e. “you can’t be too careful”.
But people have many different ideas about what it means to “be careful”. These can include the very real risks of medicalization itself. Recent stats on the negative side-effects of medical care is that 25% of all patients are harmed by unexpected side-effects of treatment or medical mistakes. Some families see that as more of a risk than the issue they are being asked to have evaluated.
This is particularly true for VBAC family who did everything their doctors and the L&D nurses ask of them, but still wound up with what they consider to be an unnecessary Caesarean. These families are hesitant at best, and some are totally unwilling, to go back into a system they have so little confidence in.
I can say with a 100% certain that every employee of the Md Bd and every representatives of the medical lobbies present at the Interested Parties meeting would strenuously object if they, or one of their children, were mandated to have medical care they didn’t want or feel they needed and had not voluntarily consented to, and most of you would hire an attorney if necessary to avoid this violation of your rights.
Ladies and gentlemen, pregnant women feel exactly the same way you do about being forced into medical care against their will. In addition, it runs 100% counter to ACOG’s own published Committee Opinions and ethical statements about the right of childbearing women.
ACOG Committee Opinions # 166 Informed Refusal & #214 Patient Autonomy: The Maternal-Fetal Relationship”

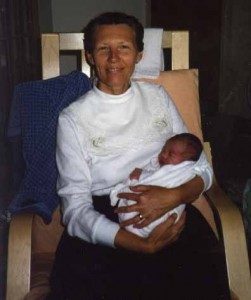
My 28-yr old grandson 26 years before he decided to go to medical school!
As the author and editor of the original SCCLM, I used ACOG’s own ethical standards for patient autonomy and the right to refuse unwanted treatment as published in ACOG Committee Opinion 166 (& 224 when developing this language for the SCCLM.
I was proud to have the policies in the SCCLM to be in alignment with ACOG’s official policies on the rights of childbearing women to decline physician recommendations and shared many of the concerns ACOG expresses about the social costs associated with any violation of individual liberty, such as forcing women into care they didn’t voluntarily consent to or boxing them into impossible choices by forcing them to decide between an unwanted repeat CS or an unattended home birth.
This ACOG document acknowledges the loss of trust in the healthcare system that not only reduces the provider’s ability to help that patient, but she will likely tell many other people about her distressing experience with the obstetrical profession and hospitals. This can’t help but affect their opinions of the healthcare system in ways that may deter them and their family members from seeking needed medical care.
ACOG Committee Opinion #214 states that:
- … medical knowledge has limitations and medical judgment is fallible. Existing methods for detection … are not always reliable indicators of poor outcome, and there is often insufficient evidence for risk-determination or risk-benefit evaluation.
- The role of the obstetrician should be one of an informed educator and counselor, weighing risks and benefits ….and realizing that tests, judgment and decisions are all fallible.
- Abiding by the patient’s autonomous decision will provide the best care for the pregnant woman and the fetus in most circumstances.
- In the event of an emergency … the obstetrician must respect the patient’s autonomy, continue to care for the pregnant woman, and not intervene against the patient’s wishes regardless of the consequences.
- When a patient’s autonomy, the woman is wronged and may be harmed, whether physically, psychologically or spiritually.
- The patient’s subsequent loss of trust in the healthcare systemmay reduce the health care provider’s ability to help her and may deter others from seeking care.
- There may be other social costs associated with this violation of individual liberty.
The SCCLM is aligns one hundred percent with ACOG’s own ethical standards for patient autonomy and the right to refuse unwanted treatment, as officially documented in ACOG Committee Opinion 166 & 224, which explicitly acknowledges and honors the rights of obstetrical patients (but obviously not midwifery patients) to decline their recommendations for treatment even if the doctor believes that they unborn or newborn baby may be harm
 Part Two:
Part Two:
“Never Events” ~ When Health Care Harms in the Context of AB 1308
The general categories of “Adverse Events” include Iatrogenic, Nosocomial, Medical Errors, and Never Events but this document focuses on “never events” in the context of midwifery and AB 1308.
Medical statisticians count the kind and frequency of medically-related “adverse events” or bad outcomes make a critical distinction btw common but untoward reaction such as unknown allergies, infection, inadvertent overdoses, wound dehiscence, etc. as opposed to what is in a category by itself known as “never events“.
“Never Events” include operating on the wrong patient, removing the patient’s only healthy kidney, prescribing the wrong drug or wrong dose, or showing up at patient’s bedside inebriated, inappropriate touching, groping or other sexual advances and other egregious breaches of professional duties and responsibilities.
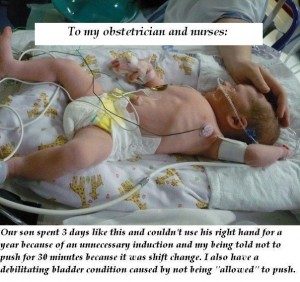
A stand-alone category of “never events” is failing to get the patient’s consent before treating them and worst of all, forcing unwanted medical care or services on informed adults who have already and repeatedly said NO.
In several important ways, ignoring this unequivocal “no” from a well-informed and mentally competent adult is one of the most egregious of all medical “never events”.
Ladies and gentlemen, this same “never event” is what ACOG insisted be included in the Licensed Midwifery Practice Act in 2013 (AB 1308). In essence, the relevant provision of AB 1308 asserts that the constitutional bedrock of self-determination and physical autonomy enjoyed by all American adults — men and women alike — be specifically and only suspended for certain categories of pregnant women who are being cared for by California licensed midwives, or they are seeking care from a Ca LM. As noted above, pregnant women receiving obstetrical care are not similarly burdered.
However, the problematic changes made to the LMPA in 2013 functionally eliminated the commonsense distinction between an actual present-tense complication and a future risk.
In virtually all other areas of healthcare, people are informed of identified risk factors and offered risk-reduction measures appropriate for their situation.
Legally and ethically, they are free to use all, none, or some of the available risk reduction-measures, but under no circumstances would they be told they were required to have a particular types of medical care and should they refuse, they would be not be allowed to access other medical services.
Under this provision of AB 1308, essentially healthy women an identified risk factor (ex. treatment for Hashimoto’s Disease) who seek or receive care from an Ca LM are functionally put in the same category as a woman with a present-tense complication, as both situations require immediate client transfer to an obstetrician and both prevent the midwife from providing any additional care until the woman has been evaluated by an obstetrician and that doctor has officially stated that the issue at hand is unlikely to “affect” the pregnancy or childbirth.
Under this provision, the pregnant woman is reduced to an inanimate object to be moved about by the midwife and the physician, even when the woman herself doesn’t believe she needs or would benefit from an obstetrical evaluation. Nonetheless this provision of AB 1309 forces her to take on significant added expense and if she lives in rural parts of the state, to face travel difficulties as many counties do not have any obstetricians. But most disturbing is the high probability that the consulting physician will protect him or herself from future malpractice litigation by routinely risking out the majority of midwifery clients they evaluate.
Prior to passage of AB 1308, the midwife had a responsibility to fully inform clients of any identified risk or medical issues (SCCLM pages 3 to 7) while the pregnant woman and her family retained their constitutional rights of autonomy and self-determination and were free to determine which risk-reduction measures and medical services they found acceptable and to decline those they did not.
‘Never events’ that would be unacceptable to healthcare providers and patients alike, and cause for disciplinary charges against the practitioners anywhere else in the healthcare system, have been institutionalized by AB 1308. Under its provisions, essentially healthy and mentally-competent adult women seeking care from licensed midwives are being systematically denied respect for their autonomy and denied constitutional right to refuse unwanted medical evaluation by an obstetrician.
This provision of AB 1308 forces these childbearing women to unnecessarily choose between unwanted medical care that is against their expressed wishes or being denied access to the care of California licensed midwives. This is the systematic imposition of “never events” have been imposed on hundreds of women over the last 7 years.
However, the continuation of these ‘never events’ is unwise, unconstitutional, immoral and unacceptable. Midwifery and consumers organizations that represent the rights and promotes a return to traditional childbirth practice for healthy women. Physiological principles and practices are also the science-based standard of care for this healthy cohort of childbearing women.
Individual midwives, childbearing women, midwifery and consumer organizations have concluded that it is up to us to stop the systematic use of these ‘never events’.
‘Never events’ have never been accepted as “OK” by the medical profession, the healthcare system, the government or the public. The legislative language provided by AB 1309 doesn’t make this “never event” any less egregious – forcing women to choose between into unwanted and for the uninsured, expensive medical services or losing access to midwifery care is wrong and in direct contradiction ACOG’s own ethical standards that clearly defines the high ground in plain language:
- Abiding by the patient’s autonomous decision will provide the best care for the pregnant woman and the fetus in most circumstances.
- In the event of an emergency … the obstetrician must respect the patient’s autonomy, continue to care for the pregnant woman, and not intervene against the patient’s wishes regardless of the consequences.
ACOG Committee Opinion #214 also identifies serious negative consequences when a patient’s autonomy is violated, noting that:
- A woman is wronged and may be harmed, whether physically, psychologically or spiritually.
- The patient’s subsequent loss of trust in the healthcare system may reduce the health care provider’s ability to help her and may deter others from seeking care.
- There may be other social costs associated with this violation.
Eliminating AB 1308’s “Never Event”
 The ethical problems created by having institutionalized ‘never events’ under AB 1308 needs to be acknowledged and corrected.
The ethical problems created by having institutionalized ‘never events’ under AB 1308 needs to be acknowledged and corrected.
The most immediate action is recognition by the Medical Board that targeting childbearing women who choose the care of midwives discriminatory and usurping their bodily autonomy and rights of self-determination is the type of extreme iatrogenic hard defined as a “never event”. All aspect of society agree that all “never events” are wrong and needs to be immediately stopped. Some people go so far as to say that stopping all varieties of “never events” is the most basic responsibility of all state medical boards.
As such, the California Medical Board should no longer file disciplinary charges against midwives that originate this provision of AB 1308 and decline to pursue any disciplinary charges already filed against Ca LMs that stem from this provision of AB 1308.
At the same time, state midwifery and consumer organizations and women’s reproductive rights groups will implement a plan to petition the state Legislature to repeal this provision from the LMPA.
Part Three: History of Midwifery Legislation in California beginning
The traditional (i.e. non-nurse practice of midwifery) and the complex issue of its legality
Midwifery legal but unregulated 1850 to first provision for licensing in 1917
Midwifery was unregulated at the time that California became part of the United States and it remain that way until 1917. That year a new provision of the Medical Practice Act created a licensing program for California midwives that required them to graduate from a midwifery training school approved by the Board of Medical Examiners (BME) and pass a midwifery board before receiving a license to practice.
BMA never approved any midwifery training programs in California so majority of licensed midwives were Japanese women who graduated from midwifery schools in Japan
Unfortunately, the BMA never approved any midwifery training programs in California but did legally recognized training school in several foreign countries including Japan, which had 27 such schools. Many of the Japanese families that emigrated to the US in the early 20th century included trained midwives who became licensed in California under the ‘reciprocity’ clause of the 1917 midwifery provision. In other cases, young Japanese-American women traveled to Japan to trained in Japanese midwifery schools. As a result, the majority of the 217 midwives licensed between 1918 and 1949 were Japanese.
MPA written so licensed midwives didn’t have exclusive right to their profession, which allowed MDs to continue providing midwifery services uninterrupted
Had the 1917 new licensing provision restricted the practice of midwifery to professionally-trained midwives, it would have meant that doctors who wanted to attend births would also have to be trained and licensed in midwifery or medical schools would have to incorporate midwifery into their regular curriculum. It’s no surprise that doctors were insulted by and rejected both of these idea. As a result, California’s first midwifery law, and all later versions of midwifery licensing (nurse-midwifery practice act in 1974 and the LMPA 1993) reiterated this idea.
These laws all say that “The license to practice midwifery does not authorize the holder to practice medicine or surgery“. However, nothing in the MPA prevents physicians from providing what essentially are midwifery services — attending the births of healthy women with normal pregnancies and the medical school curriculums do not include any classes on theprinciples and practices of physiologically-managed normal childbirth.

Japanese Internment Camp in California – 1941-1945
Presidential Executive Order 9066 ~ Internment of Japanese Midwives followed by SB 966 — repeal of midwifery licensing
Early in the WWI, presidential Executive Order 9066 resulted deported of the entire California population Japanese citizens to internment camps, a circumstance well-documented in the Board of Medical Examiners’ annual Directory of Licentiates. After the WWII ended, the BME and unidentified individuals or groups sponsored SB 966, a bill to repeal California’s midwifery licensing law. SB 966 permitted already licensed midwives to continue to practice but prevented any additional licensing of traditional of “non-nurse” midwives in our state.
Introduction of 7 midwifery licensing bills in the State legislature between 1977 and 1993
Unknown to the 1949 Legislature, the effect of SB 966 would be introduction of 7 midwifery licensing bills in the State legislature between 1977 and 1993. There were two reason for this.
California Medical Practice Act never identified midwifery as an illegal activity
First, the 1876 Medical Practice Act itself, and all subsequent amendments passed during the following two hundred years, didn’t mentioned either childbirth or midwifery or in any direct way identified midwifery as an illegal activity. While the 1917 provision provided for licensure, the new midwifery law did not include the usual exclusive entitlement to the practice of midwifery that applies to all other healthcare professions (i.e. its legal for non-midwives to practice midwifery).
 attorneys defined the lay practice of midwifery
attorneys defined the lay practice of midwifery
As for the long-term effect of SB 966, a number of attorneys defined the lay practice of midwifery as no longer regulated but also not outlawed, what they described as a “grey area of law”.
Since state licensed midwives were no longer available in California, the lay practice of midwifery was grew each year. By the early 1980, the California Department of Consumer Affairs estimated that as many as 500 lay midwives were practicing in the state.
The second reason was the 1973 arrest of three Santa Cruz midwives by the Board of Medical Quality Assurance (BMQA) who charged them with the crime of practicing medicine without a license. The criminal case of the People vs. lay midwife Alice Katherine Bowland went to the State’s Supreme Court in 1976.
The Bowland Decision adjudicated two different but fundamentally interdependent questions – (a) did childbearing women in California have a legally-established right to choose the “manner and circumstances” of normal childbirth and (b) was the lay practice of midwifery an illegal practice of medicine under the State’s Medical Practices Act?
Relative to a childbearing woman’s rights to “alternative” form of childbirth services, the Justices noted that the State’s Legislature had never “gone so far” as to guarantee the right of autonomy and self-determination for childbearing women in California and identified this to be a matter for the Legislature and not the Courts. With this as background, the Supreme Court ruled that California mothers did not have the right to choose a lay midwife.

As noted earlier, the California Medical Practice Act had no direct reference to childbirth or midwifery (i.e. the words “childbirth” and “midwifery” never appear aside from the 1917 provision) but the Bowland Count focused on a phrase in the B&P section 2141 (now sec. 2052) that listed “unlawful practices” for persons not holding a California medical licensed to include diagnosing, treating, operating or prescribing “for any affliction, blemish, deformity, disease, disfigurement, disorder, injury or other mental or physician condition”.
The California Supreme Court acknowledged that normal childbirth per se was not an activity forbidden by the “unlawful practices” section of the MPA.
However, the Justices concluded that the Section 2141 phrase “or other mental or physical conditions” at the end of the seven descriptive words referring to pathological conditions applied to the legal issue of lay midwifery made the practice of lay midwifery illegal because pregnancy was obviously a “physical condition”, therefore it “treatment” by lay midwives constituted an unauthorized and thus an illegal practice of medicine.
Since publication of this California stare decisis in 1976 a handful of attorneys that had no previous interest in childbirth or connection with midwives or midwifery opined that the Bowland Decision was smacked of a pre-loaded solution looking for a problem. They based this opinion on the acrobatic contortions required to define pregnancy as a proscribed condition within the meaning of the MPA and to define the care of healthy childbearing women by midwives to represent an illegal “treatment”.
The first direct-entry midwifery licensing bill was introduced in the California Legislature in 1977, followed by 5 more bills over the next two decades that were quickly and effectively killed in committee by organized medicine. In the early 1990s, Senator Killea, who had voted for bills that supported women’s reproductive rights, became interested in carrying midwifery legislation. In addition to licensing she wanted to see legislation that would guarantee the rights of childbearing women to choose the manner and circumstance of normal childbirth, including the choice of community-based midwifery care.
This was a direct result of the historical ruling by the Bowland Court — that healthy women in California did not have the right to choose “alternative” childbirth care — and the remark by the Justices’ remark about a legislative remedy. So Senator Killea agreed to carry a midwifery bill that would provide a legislative foundation for a woman’ right to determine the “circumstance” if normal childbirth, including the right to be cared for by a professionally trained and state-licensed midwife.
 Senator Killea’s legislative efforts need to be seen in the wider context of her life prior to being elected to the California Legislature. During World War II she worked for the US Office of Strategic Services as a professional intelligence officer stationed in Europe and involved in undercover missions. After returning to the States at the end of the war, she and her husband Jack Killea were the second and third persons appointed by then President Truman to create the Central Intelligence Agency (CIA) in 1947.
Senator Killea’s legislative efforts need to be seen in the wider context of her life prior to being elected to the California Legislature. During World War II she worked for the US Office of Strategic Services as a professional intelligence officer stationed in Europe and involved in undercover missions. After returning to the States at the end of the war, she and her husband Jack Killea were the second and third persons appointed by then President Truman to create the Central Intelligence Agency (CIA) in 1947.
Obviously, Senator Killea was no slouch when it comes to understanding the big picture and its many complexities, including the historic tension between midwifery and powerful special interest groups that have permanently opposed the practice of midwifery for more than a century.
As a former intelligence officer during the world war in Europe, Senator Killea was trained to tolerate the serious and even life-threatening risks that went along with her important job. It also meant being rough and tough and hard to bluff, which is an excellent preparation for carrying midwifery legislation, which really takes guts. These senatorial authors immediately find the big guns of organized aimed at their forehead as a flood of campaign contributions to their political opponent in an orchestrated effort to keep them from getting re-elected. This is way most people with political aspiration would not be willing to throw it all away by carrying a bill supporting midwifery.
 But there is another part of Senator Killea story that had deeply personal and painful consequences but also was very influenced in her support for the rights healthy women to directly control their own reproductive lives.
But there is another part of Senator Killea story that had deeply personal and painful consequences but also was very influenced in her support for the rights healthy women to directly control their own reproductive lives.
As a seated member of the state senate, Senator Killea voted against bills that would have eliminated access to safe and legal abortion services and voted in support of bills that protected women’s reproductive rights, including access to safe and legal abortion services. As a result, Senator Killea, an observant and life-long Catholic was excommunicated by the Catholic bishop of her diocese.
After collaborating with childbearing women, families and practicing midwives, Senator Killea introduced SB 350 in the spring of 1993 and the Licensed Midwifery Practice Act was passed that fall.

Ina May Gaskin, Grand Dame of Midwifery in America!
The LMPA, in combination with its first 3 amendments, provided the legal basis for mentally-competent adult women to choose a state-licensed midwife. The LMPA allows essentially healthy childbearing women with normal pregnancies to labor, and if everything remains normal, give birth in a non-medical setting, such as community birth centers and the family’s home, under the care of a licensed midwife.
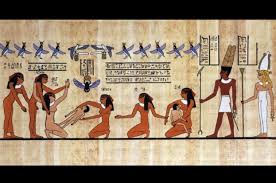 Five thousand year-old Egyptian hieroglyphics have memorialized midwifery as the first and the oldest form of organized healthcare service. The lives and practices of midwives are record in many places in the Judeo-Christian Bible.
Five thousand year-old Egyptian hieroglyphics have memorialized midwifery as the first and the oldest form of organized healthcare service. The lives and practices of midwives are record in many places in the Judeo-Christian Bible. We learn about pregnancy and childbearing from inside our own bodies, as a series of direct experiences. This not only includes biological sensations but also the psychological aspects of childbearing, such as its ‘normal’ anxieties, emotional ups and downs and the extraordinary feeling when we push our baby out under our own power!
We learn about pregnancy and childbearing from inside our own bodies, as a series of direct experiences. This not only includes biological sensations but also the psychological aspects of childbearing, such as its ‘normal’ anxieties, emotional ups and downs and the extraordinary feeling when we push our baby out under our own power!
 Historically, this was not true for midwives. According the demographic research spanning several centuries and many different countries, the “average” midwife begins by apprenticing with an older experience midwife when the apprentice’s youngest child was at least 10 or more years old. The average length of an apprenticeship was about 10 years, so most of women did not begin practicing independently until they were in their forties or even older.
Historically, this was not true for midwives. According the demographic research spanning several centuries and many different countries, the “average” midwife begins by apprenticing with an older experience midwife when the apprentice’s youngest child was at least 10 or more years old. The average length of an apprenticeship was about 10 years, so most of women did not begin practicing independently until they were in their forties or even older.
 The case for midwifery
The case for midwifery Midwifery is “skilled, knowledgeable and compassionate care for childbearing women, newborn infants and families across the continuum throughout pre-pregnancy, pregnancy, birth, postpartum and the early weeks of life. Core characteristics include optimizing normal biological psychological, social, and cultural processes of reproduction and early life; timely prevention and management of complications; consultation with and referral to other services; respect for women’s individual circumstances and views, and working in partnership with to strengthen women’s own capabilities to care for themselves and their families.” Lancet Series on midwifery (June 2014).
Midwifery is “skilled, knowledgeable and compassionate care for childbearing women, newborn infants and families across the continuum throughout pre-pregnancy, pregnancy, birth, postpartum and the early weeks of life. Core characteristics include optimizing normal biological psychological, social, and cultural processes of reproduction and early life; timely prevention and management of complications; consultation with and referral to other services; respect for women’s individual circumstances and views, and working in partnership with to strengthen women’s own capabilities to care for themselves and their families.” Lancet Series on midwifery (June 2014).
 The case for midwifery: the potential of midwives for improving quality of care
The case for midwifery: the potential of midwives for improving quality of care References
References
 Medical Board of California
Medical Board of California
 Obviously we have very different experiences of our respective professions, but around the world childbirth is the very safest when midwives are a normal part of the mainstream healthcare system, women receive maternity care during pregnancy and physiological management of childbirth is the evidence-based standard of care for healthy women with normal pregnancies, and midwives and obstetricians have a mutually cooperative and respectful relationship with each other.
Obviously we have very different experiences of our respective professions, but around the world childbirth is the very safest when midwives are a normal part of the mainstream healthcare system, women receive maternity care during pregnancy and physiological management of childbirth is the evidence-based standard of care for healthy women with normal pregnancies, and midwives and obstetricians have a mutually cooperative and respectful relationship with each other. Risk Factors, Risk-Reduction Measures, Informed Consent, the Midwife’s Responsibilities and Client’s Rights
Risk Factors, Risk-Reduction Measures, Informed Consent, the Midwife’s Responsibilities and Client’s Rights
 Part Two:
Part Two: The ethical problems created by having institutionalized ‘never events’ under AB 1308 needs to be acknowledged and corrected.
The ethical problems created by having institutionalized ‘never events’ under AB 1308 needs to be acknowledged and corrected.

 Senator Killea’s legislative efforts need to be seen in the wider context of her life prior to being elected to the California Legislature. During World War II she worked for the US Office of Strategic Services as a professional intelligence officer stationed in Europe and involved in undercover missions. After returning to the States at the end of the war, she and her husband Jack Killea were the second and third persons appointed by then President Truman to create the Central Intelligence Agency (CIA) in 1947.
Senator Killea’s legislative efforts need to be seen in the wider context of her life prior to being elected to the California Legislature. During World War II she worked for the US Office of Strategic Services as a professional intelligence officer stationed in Europe and involved in undercover missions. After returning to the States at the end of the war, she and her husband Jack Killea were the second and third persons appointed by then President Truman to create the Central Intelligence Agency (CIA) in 1947. But there is another part of Senator Killea story that had deeply personal and painful consequences but also was very influenced in her support for the rights healthy women to directly control their own reproductive lives.
But there is another part of Senator Killea story that had deeply personal and painful consequences but also was very influenced in her support for the rights healthy women to directly control their own reproductive lives. At the November 2019 Quarterly meeting of the California Medical Board of California as agenda item (11-B) was formally proposing that the Board carry a bill that would make it illegal for Ca LMs to provide care VBAC care.
At the November 2019 Quarterly meeting of the California Medical Board of California as agenda item (11-B) was formally proposing that the Board carry a bill that would make it illegal for Ca LMs to provide care VBAC care.
 Editor’s Note — there are a few places in this draft that are still unfinished, but so far i haven’t been able to find the final version submitted to the MBC on that date.
Editor’s Note — there are a few places in this draft that are still unfinished, but so far i haven’t been able to find the final version submitted to the MBC on that date.
 When is a Risk a RISK?
When is a Risk a RISK? I am one of the few individuals in either the midwifery community or the employ of the Medical Board who has been involved full-time in the legal and legislative issues of California midwifery before, during and after the passage of the 1993 LMPA.
I am one of the few individuals in either the midwifery community or the employ of the Medical Board who has been involved full-time in the legal and legislative issues of California midwifery before, during and after the passage of the 1993 LMPA.


 Quotable materials on theutter failure of policy mandating use of continuous EFM on healthy women with normal pregnancies and it’s high human and economic costs
Quotable materials on theutter failure of policy mandating use of continuous EFM on healthy women with normal pregnancies and it’s high human and economic costs THE MEDICAL BOARD OF CALIFORNIA
THE MEDICAL BOARD OF CALIFORNIA