Easy to share link https://tinyurl.com/bmezd79k
 The case for midwifery
The case for midwifery
Related links
- Infographic: case for midwife-led continuity of care
jpg, 336kb - WHO’s work on quality midwifery care for mothers and newborns
- Midwives’ voices, midwives’ realities report 2016
- More publications on midwifery
What is midwifery?
 Midwifery is “skilled, knowledgeable and compassionate care for childbearing women, newborn infants and families across the continuum throughout pre-pregnancy, pregnancy, birth, postpartum and the early weeks of life. Core characteristics include optimizing normal biological psychological, social, and cultural processes of reproduction and early life; timely prevention and management of complications; consultation with and referral to other services; respect for women’s individual circumstances and views, and working in partnership with to strengthen women’s own capabilities to care for themselves and their families.” Lancet Series on midwifery (June 2014).
Midwifery is “skilled, knowledgeable and compassionate care for childbearing women, newborn infants and families across the continuum throughout pre-pregnancy, pregnancy, birth, postpartum and the early weeks of life. Core characteristics include optimizing normal biological psychological, social, and cultural processes of reproduction and early life; timely prevention and management of complications; consultation with and referral to other services; respect for women’s individual circumstances and views, and working in partnership with to strengthen women’s own capabilities to care for themselves and their families.” Lancet Series on midwifery (June 2014).
Who is a midwife?

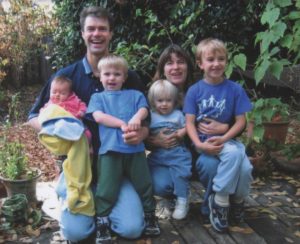
Alison Price, Ca LM, San Francisco, Ca
A midwife is a person who, having been regularly admitted to a midwifery educational programme, duly recognized in the country in which it is located, has successfully completed the prescribed course of studies in midwifery and has acquired the requisite qualifications to be registered and/or legally licensed to practice midwifery. (ICM 2005)
Who is a skilled birth attendant
A skilled birth attendant is an accredited health professional — such as a midwife, doctor or nurse — who has been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies, childbirth and the immediate postnatal period, and in the identification, management and referral of complications in women and newborns. (WHO/ICM/FIGO 2004)
 The case for midwifery: the potential of midwives for improving quality of care
The case for midwifery: the potential of midwives for improving quality of care
- 83% of all maternal deaths, stillbirths and newborn deaths could be averted with the full package of midwifery care (including family planning);1
- 62% of effective practices within the scope of midwifery show the importance of optimising the normal processes of childbirth and early life, and empowering women to care for themselves and their families;2
- 56 maternal and neonatal outcomes where found to be improved through midwifery practice and philosophy of care;2
- 87% of service need can be delivered by midwives, when educated to international standards;3
- 82% reduction in maternal mortality possible with universal midwifery coverage;1
- Midwifery is associated with more efficient use of resources and improved outcomes when provided by midwives who are educated, trained, licenced and regulated in international standards2. Midwifery is a ‘best buy’ investment;3
- Midwifery is associated with reduced maternal and neonatal morbidity, reduced interventions in labour, improved psycho-social outcomes and increased birth spacing and contraceptive use;4
- Community based midwives have been found to rank positively for economy, efficiency and effectiveness;4
- Midwifery should be considered a core part of universal health coverage. Quality midwifery care is central to achieving national and global priorities and securing the rights of women and newborn infants;4
- Quality relates to the right for women and newborns to the highest standard of health and is synonymous with women-centred care. Providing quality care is most efficient through midwifery care for all childbearing women;5
- There were no adverse outcomes associated with midwife-led care but significant benefits, thus it is recommended that all women should be offered midwife-led continuity models of care;5
- Case loading midwifery care is safe and cost effective;6
- Midwives have the potential to provide excellent quality of care but socio-cultural, economic and professional barriers must be overcome to allow them to practice to their full potential.7
 References
References
1 Homer, CS, Friberg, IK, Dias, MA et al. “The projected effect of scaling up midwifery”. Lancet. 2014;384: 1146–1157
2 Renfrew, MJ, McFadden, A, Bastos, MH et al. “Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care”. Lancet. 2014; 384: 1129–1145
3 UNFPA ICM, WHO: “The state of the world’s midwifery 2014: A universal pathway. A women’s right to health”. 2014, New York: United Nations Population Fund
4 Sandall J, Soltani H, Gates S, Shennan A, Devane D. “Midwife-led continuity models versus other models of care for childbearing women”. Cochrane Database of Systematic Reviews 2016, Issue 4
5 Ten Hoope-Bender P, de Bernis L, Campbell J et al (2014). “Improvement of maternal and newborn health through midwifery”. Lancet. 2014;384: 1226-35
6 Tracy SK, Hartz DL, Tracy MB, Allen J, Forti M, Hall B, White J, Lainchbury A, Stapleton H, Beckmann M, Bisits A, Homer C, Foureur M, Welsh A, Kildea S: “Caseload midwifery care versus standard maternity care for women of any risk: M@NGO, a randomized controlled trial”. Lancet 2013,382:1723–1732.
7 Filby A, McConville F, Portela A (2016) “What Prevents Quality Midwifery Care? A Systematic Mapping of Barriers in Low and Middle Income Countries from the Provider Perspective”. PLoS ONE.11(5)

https://www.who.int/maternal_child_adolescent/topics/quality-of-care/midwifery/case-for-midwifery/en/#:~:text=Midwifery%20is%20%22skilled%2C%20knowledgeable%20and,the%20early%20weeks%20of%20life.
You must log in to post a comment. Log in now.