https://tinyurl.com/ybvde6cx ~ This URL links to Parts 1. You can access Part 2 by clicking the link at the bottom of Part 1.
The story behind the 1993 Licensed Midwifery Practice Act and organized medicine’s 2013 amendment to the LMPA that irrationally restricts access to care by Ca LMs
The California Licensed Midwifery Practice Act was introduced in 1993 by Senator Lucy Killea specifically to reduce the risks that pregnant women and their unborn/newborn babies face when the mother-to-be does not receive quality maternity care and the associated complications of “no care” which includes an increase in premature births, undetected pregnancy complications for either mother or unborn baby, and the dangers of unattended births.
Whether planned or unplanned, not having prenatal care and not having a trusted and skilled birth attendant present during labor and birth drastically increases the danger to mothers and babies both.
Lack of prenatal care is associated with a dramatic increase in the rate of prematurity. Hospital caring for premature babies can be as much as a million dollars per infant and often includes expensive long-term disabilities. Treatment of newborns with respiratory-related difficulties, which is a major problem for premies, is the *very most expensive* type of hospital care — even more frequent and expensive than treating spinal cord injuries and 3rd-degree burns.
More than half of the hospital expense for pre-term babies is billed to the State’s MediCal program. Under dire circumstances, even high-income families come to depend on this state-federal program to pay for neonatal intensive care when the parents’ private insurance maxes out. Unfortunately, the problems associated with a premature birth do not end when the baby is discharged from the hospital. While the negative effects of pre-term birth fall heaviest on parents and child, there are also expensive downstream problems for our schools and other hidden or long-term costs to society.
As for the risks of unattended birth, they are obvious and also expensive, both in treasure and human tragedy.
The Legislative Intent of SB 350 was to mitigate these problems by better serving the needs of families who couldn’t find afford conventional maternity care and/or wanted to avoid the highly medicalized and interventive hospital care that is the current standard in the US. These families were seeking a reasonable, safe and lawful alternatives, including care by midwives trained to support the physiology of normal childbirth in a non-medical setting — the family’s home or free-standing birth centers staffed by professional midwives and family practice physicians.
Why Nurse-Midwifery Was/Is Not an Answer

Certified Nurse-Midwife, Kate Bowland (standing) & provider of planned home birth services in Santa Cruz County for 45 years (Yea Kate!)
Prior to passage of the LMPA in 1993, California law only legally recognized the practice of certified nurse-midwives (the Nurse-Midwifery Act of 1974). However, each CNM is only permitted to provide midwifery services if an obstetrician is willing to enter into a written contract with her to legally “supervise” them.
Unfortunately, the 1974 nurse-midwifery licensing law does not require that any California-licensed obstetrician actually supervise a nurse-midwife.
As an additional disincentive to the practice of nurse-midwifery, the legal supervisory role of obstetricians means doctors can be held liable for care provided by the nurse-midwife if there is a malpractice suit. Obviously, their professional liability insurance carriers do not allow them to do this.
The obstetrical profession has always seen midwifery as a competing profession and economic threat. So it’s no surprise that 99.99% of California obstetricians refuse to take on the onerous responsibility for one of their competitors. With rarest of exceptions, the few who do agree to supervise a nurse midwife insisted that she only attend hospital births, which required the midwife to abide by obstetrical department protocols (instead of physiologically-based practices).

Standard obstetrical protocols for hospital delivery, with the mother lying on her back on a delivery room table, buried under sterile drapes in an anti-gravitational position while trying to push her baby uphill while her obstetrician, L&D and nursery nurses, several medical students and other hospital personnel look on.
In 1976, families who were hoping to receive community-based midwifery care from a state-licensed CNM were dismayed to discover that the new law was obviously unworkable and did not allow this so these frustrated families sought out the services of lay midwives. However, if they were unable to locate a suitable birth attendant in their geographical area, they often opted for an unattended birth. This was such an obviously dangerous problem that Jerry Brown, during his first term as governor (1975-83), became personally involved in supporting a new, non-nurse midwifery licensing law.
Governor Brown’s administration described the impasse over mandatory supervision of midwives by obstetricians as “structural barriers to practice” inserted by organized medicine into the 1974 nurse midwifery bill. This prevented nurse-midwives from providing services to low-income women and families seeking alternative care, which was the major purpose of the licensing law. The nurse-midwifery law was also supposed to greatly reduce the cost of maternity care being paid by the State’s MediCal program, but the unworkable physician supervision clause rendered that useless as well.
In 1976, Gov. Brown directed the California Department of Consumer Affairs (the DCA is a state agency under the control of the executive branch) to actively support passage of a new, non-nurse midwifery-licensing law [AB 1896] as an independent discipline that was not under the control of the medical profession (which unfortunately is still the case for California nurse-midwives 54 years later).

During this period of time, three midwifery licensing bills (AB 1896, AB??, SB??) were introduced and promoted by the Governor Brown’s office and Mr. Michael Krisman, Deputy Director of the Department of Consumer Affairs**.
Unfortunately, the lobbying efforts of organized medicine were able to overrule even the direct support of Governor Brown and the DCA. Altogether, there were six attempts to pass a non-nurse (direct-entry) midwifery licensing law between 1976 and 1993 failed.
{** See the Department of Consumer Affairs’ 11-page document written by Deputy Michael Krisman September 8, 1977 entitled AB 1896 – BACKGROUND INFORMATION PAPER ~ THE MIDWIFERY PRACTICE ACT OF 1978
DCA’s pro-active support of a new mfry licensing law included creating the original “Midwifery Advisory Council” in 1981. Lay midwives (including myself) and many grassroot activists met regularly in the Capitol building in a conference room provided by the DCA to work on midwifery legislation that would allow state-licensed nurse AND non-nurse midwives (as a combined legal category) to be reimbured by MediCal when providing care to eligible low-income families.
In 1981 & 1983 public hearing were held in northern and southern parts of the State. These Alternative Birth Hearings were chaired by State Senator John Vasconcellos and Mr. Jack Winters (Editor’s note-2-self: Janet Ashford to may remember names & other details and still have newspaper clippings).
Senator Lucy ~ Author of the LMPA and Heroine to the State’s childbearing families and direct-entry midwives
When the overwhelming odds against passage of a non-nurse midwifery law are taken into account, Senator Lucy Killea’s offer to author and vigorously, personally promote SB 350 can be seen as the brave and bold move it really was. Senator Killea was a remarkable woman with an extraordinary history of public service.
During WWII she was employed by the US military in Europe as an “operative” (i.e. a spy). At the end of WWII, she and her new husband Jack Killea were the second and third people hired by then-President Harry Truman to run the newly authorized Central Intelligence Agency (CIA).
Senator Killea was also the only member of the Legislature to be denied communion by the Catholic Bishop of her San Deigo parish church in retaliation for her vote to decriminalize abortion. So her effort to find an alternative solution to the problems created by the historical domination of all childbirth services in the State by organized medicine over a period of 54 years was in line with her illustrative record of personal courage and ethical standards translated into protective public policy.
The intent of SB 350 was to professionalize non-nurse midwifery and ultimately improve maternal-infant outcomes in California. The ancillary goal of the LMPA was to reduce the State’s share of expense thru the MediCal program that was associated with a high rate of prematurity and childbirth-related complications resulting from a lack of access to maternity care and unattended births.
The LMPA passed the California Legislature unanimously and was signed into law by the governor on October 11, 1993. In 2016, there were more than 400 midwives licensed in California under the LMPA and over 3,000 babies born in non-medical settings (birth centers and family residence) under their care. **Licensed Midwives Annual Report (LMAR-2016)
SB 1479 ~ An Important & Clarifying Amendment to the LMPA by Senator Liz Figueroa
The LMPA was first amended in the year 2000 by Senator Liz Figueroa. SB 1479 stated as a matter of California state law that childbirth was a normal aspect of biology and not a medical disease. SB 1479 legally clarified the characteristics of physiological management and the supportive, non-interventive practices associated with the community-based practice of midwifery, which is a non-medical (in the sense of non-allopathic) discipline legally distinct from the allopathic practice of obstetrics.
By California law, the licensed midwifery model of care includes:
- Informed choice
- Continuity of individualized care
- Sensitivity to the emotional and spiritual aspects of childbearing
- Monitoring the mother throughout the childbearing cycle including
her physical, psychological, and social well-being - Providing individualized education, counseling, and prenatal care
- Continuous hands-on assistance during labor and delivery
- Postpartum support
- Minimizing technological interventions
- Identifying and referring women who require obstetrical attention

Hour-old baby boy in a “bunny bag” — a midwife’s invention that is a tiny sleeping bag made from cloth diapers and super absorbent microfiber fabric. It helps keep newborns warm while being held by family members, who often have a hard time keeping the baby covered and warm
In the year 2000, this amendment to the LMPA formally acknowledged the right of essentially healthy pregnant women to exercise self-determination in regard to normal childbirth. This was an affirmative response by the Legislature to a legal issue raised by California Supreme Court in the Bowland Decision.
In 1976 the Bowland Court ruled that childbearing women had no intrinsic right to make decisions about the type of care they received during pregnancy and childbirth, noting that the California Legislature had “never gone so far” as to acknowledge that, as a class, healthy childbearing women in California had the right to choose “the manner and circumstances of normal childbirth”.
It should be noted that the Bowland Count did not rule say that childbearing women couldn’t legally decline prenatal care during pregnancy or plan to have an unattended birth. They just noted that the Legislature had never affirmed a pregnant woman’s right to choose a maternity care provider that was OTHER than conventional hospital-based obstetrical providers.
The Legislative Intent of SB 1479 rectified this oversight, acknowledging that in California:
(b) Every woman has a right to choose her birth setting from the full range of safe options available in her community
(e) The midwifery model of care is an important option within comprehensive health care for women and their families and should be a choice made available to all women who are appropriate for and interested in home birth.
This provides legislative authority for the practice of traditional (i.e. non-physician) birth attendants and the choice by parents of tradition/alternative (out-of-hospital) locations.
In 2002, SB 1950 (Figueroa) mandated that a regulation be promulgated that would define a midwifery standard of care for California licensed midwives). This amendment resulted in the approval of the Standard of Care for California Licensed Midwives (SCCLM) by the California Medical Board in September 2005 and its formal adoption the Office of Administrative Law (OAL) in the regulatory code March 6, 2006.
In 2006, SB 1638 (Figuroa) directed the California Medical Board to create a Midwifery Advisory Council composed equally of Ca LMs and consumers. The Council meets 3 or 4 times a year and currently has 6 members. Advisory Council meetings are now webcast for public viewing and those videos are archived for reference at a later time by the public.
SB 1638 also mandated that the MBC develop an administrative process for the annual collections of statistics for all licensed midwives to be reported and collated by OSHPD (Licensed Midwives Annual Report) and formally reported by the Medical Board to the State Legislature each year.
Starting in 2007, the LMAR has tracked the number of families that received care from Ca LMs each year and standard maternal-infant statistical outcomes. These include the number of normal vaginal birth attended in an out-of-hospital setting, number of hospital transfers and all sub-optimal outcomes, including Cesarean deliveries and any serious morbidity within first 6 weeks and mortality. These online annual reports have been available to the public since 2010.
 I cannot stress enough that all these changes were sought out by practicing midwives and consumer groups, especially the California Association of Midwives (CAM) and California Families for Access to Midwives (C-FAM).
I cannot stress enough that all these changes were sought out by practicing midwives and consumer groups, especially the California Association of Midwives (CAM) and California Families for Access to Midwives (C-FAM).
We all worked hard and spent organizational funds to find a legislator willing to sponsor these amendments. After this critical stage was accomplished, professional and advocacy groups as the office staff of the two Legislator’s offices (special thanks to Liz Smith and Vincent Marchand in Sen. Figueroa’s office 2000-2006) We all burned the midnight oil to push these bill through.
Licensed midwives and consumer groups worked for changes in the LMPA that would mandate annual reporting by each practicing midwife, who would be required to provide a great many details about the care provided, including any bad outcomes. We believed that legislation mandating the Medical Board to host a Midwifery Advisory Counsel would dramatically improve the professional relationship between licensed midwives and our regulatory agency (MBC). Indeed, this has greatly improved relationship btw our regulatory agency and its midwife licentiates.
In an on-going effort to make midwifery the best it can be, the 1993 LMPA and its first 3 amendments allowed the profession of licensed midwifery to further fine-tuning the care it lawfully provides to childbearing families in California seeking alternative childbirth services that are lawful, safe, cost-effective and able to reduce the likelihood that the laboring woman and her newborns would be exposed to risky and unwanted medical and surgical interventions.
The problem is NOT Senator Killea’s midwifery licensing law, but the continued LACK of access to high-quality maternity care and midwifery services caused by inappropriate amendments to the LMPA sponsored by special interest groups
Whatever people may think of community-based midwifery, they should be reassured by the following facts:
The public health problems surrounding normal childbearing in California are not the result of the care by state-licensed midwives, but the preventable danger to pregnant women and their unborn babies when they don’t get regular prenatal care and are forced to chooe between the Devil and he Deep Blue Sea — eiher an unwanted hospial birth (or in some cases, an unwanted Cesarean) of have an unattended birth and attendant risks
The combination (no prenatal care-unattended labor, birth and neonatal period) has 20 to 40-fold increase in mortality of mothers and unborn/newborn babies. One study of unattended births in a religious group in Indiana identified 6 maternal deaths out of 344 births or 1 mother and 21 stillborn or newborn babies for every 57 births. (Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31: ~ see abstract at end of this document)
 Preventing Needless Childbirth Tragedies
Preventing Needless Childbirth Tragedies
The tragedies cited in the study above were all “preventable” deaths due to untreated hemorrhage in new mothers and untreated infection in neonates. Obviously, the basic issue in these cases was a regrettable (and I believe an uninformed) choice made by these families to eschew prenatal care and having a trained birth attendant present during labor and birth, as well as refusing to use medical and emergency services in the face of life-threatening complications.
But these high maternal-infant mortality statistics are a grizzly testament to just how successful midwifery care is at preventing such tragedies.
As attested to by the last 10 years of data collected by the California Licensed Midwives Annual Report (thank you Senator Figeroa!), we know the majority of unexpected problems associated with childbirth can be prevented or successfully managed when professionally-licensed midwives are authorized to:
- Provide prenatal care with regular risk-screening and referrals to medical services as needed
- Physically examine and evaluate the health status of the pregnant woman and her unborn fetus prior to the term onset of active labor (late pregnancy, very early labor), so those with complications can be prophylactically transferred to medical services
- Be present during the mother’s active labor, the birth of her baby and immediate postpartum-neonatal period and the 6-week of follow-up care for both mother and baby, which also includes hospital transfer and/or use of emergency medical services as needed
But starting in 1949, when the original 1917 midwifery licensing law was repealed by the California Legislature at the request of the medical community, no such safeguards were legally available in California until the passage of the LMPA in 1993. During that 44-year gap, California families had only two legally-recognized options:
(a) “no care” – i.e. no prenatal care; unattended birth; delayed access to emergency medical services when needed
(b) medicalized obstetrical care that is often experienced by laboring women and their families as similar to being in intensive care unit (ICU).
If those two extremes — “no care” and highly medicalized, expensive hospital-based obstetrical care for healthy women — met the needs of 100% of childbearing women in California, there would have been no need for the Legislature to ever create the new category of professionally-licensed direct-entry midwifery.
Unfortunately for the special interest groups who supported the status quo between 1917 and 1993, the actual facts belie any assumption these two extremes were able to meet the needs of the childbearing public or the fiscal responsibility of the State’s MediCal program to pay for the maternity care of eligible low-income families.
Compelling evidence in more recent times that a state-sanctioned category of professional non-nurse midwives was necessary is unanimous passage by the California State Legislature of the original Licensed Midwifery Practice Act of 1993 (SB 350) and three (SB 1479, SB 1950, and SB 1638 – Sen. Figueroa) of its four amendments.
As the risk of being redundant, the incontrovertible facts are both plain and simple: The presence of a trained midwife, like that of a lifeguard at the pool, always makes childbirth orders-of-magnitude safer for childbearing women and their unborn and newly born babies.
That means providing the option of professional midwifery care to low-income women, socially and religiously conservative families, ethnic groups that prefer traditional forms of midwifery care, and families that, for a great variety of valid and rational reasons, want or need an alternative to highly-medicalized hospital obstetrics. Since 1993, the answer to what otherwise would be insurmountable problems had been the LMPA.
Midwifery Licensing and its Important Contribution to Childbearing Families
Passage of the LMPA in 1993 legally acknowledged and preserved the traditional arts of midwifery within the context of modern medical science and evidence-based “best practices”. Through formal education and clinical training, over 400 California licensed midwives have had the opportunity to incorporate the historic quality of traditional midwifery care with the “best practices” of modern medicine.
If a medical problem should occur in an out-of-hospital setting (home or birth center), midwives are scientifically trained first-responders able to provide effective emergency interventions, and refer or transfer mother or baby to medical providers whenever necessary. As noted earlier, this reduces risks during pregnancy, and the frequency and severity of preventable childbirth complications, making normal childbirth in healthy women both *safer* and more cost-effective.
2013 ~ Hostile taker-over by organized medicine is a disguised restriction on midwifery services and denial-of-service to healthy childbearing women
Unfortunately, the fourth amendment to the LMAP represents a ‘hostile take-over’ — AB 1308 was sponsored by lobbyists representing organized medicine in 2013. This amendment, which was negotiated by lobbyists for ACOG, drastically reduced the scope of practice for direct-entry midwives and the number of essentially healthy childbearing women that California licensed midwives can legally provide services to.

Prior to its passage, the LMPA the scope of practice for CaLM was defined as providing routine prenatal care, risk-screening, and normal childbirth services to women with no evident medical, obstetrical or perinatal complications. Only if a pregnant or laboring woman or newborn developed a clinically significant complication did the LMPA mandate obstetrical care or transfer to hospital-based services. This logical and common sense provision of the law was fully supported by parents, midwives, the medical profession and the general public as an appropriate safety measure. Unfortunately, AB 1308 changed that for the worse.
AB 1308 also directly repealed the California Licensed Midwives Standard of Care and specifically negated our Standard of Care’s policy statement on the licensed midwife’s ethical duty to inform and recommend physician consultation in relation to all identified risk factors, and simultaneously denied the childbearing woman’s right to self-determination (i.e. Patients Rights), including the right to decline obstetrical referrals and evaluations in relation to certain risk factors.
AB 1308 eliminated the childbearing family’s right of self-determination and informed consent/refusal, while dramatically increasing the number of childbearing families that now don’t “quality” for midwifery services under the LMPA.
I believe this provision is unconstitutional under both state and federal law.
The legal theory of ‘Adherence’ ~ a shield for midwives and mothers
AB1308 this violates a legal theory described as “adherence“. This describes a logical expectation that a law or set of laws relating to the same general theme has an internal integrity. New laws or novel interpretations of provisions in an existing law that violates that integrity risk being struck down by the Courts. For example, if a law developed to protect minor children is being implemented in ways that predictably increased the level of danger experienced by minor children, those actions would be found to violate the basic intention of the law based on the theory of “Adherence’.
 The legislative intent and provisions of the LMPA and three of its four amendments all materially enhance a midwifery licensing law whose purpose is identified in the “Legislative Intent” as making childbirth safer. The LMPA was to design to achieve these goals by creating a legally-defined mechanism to professionally train and license non-nurse/direct-entry midwives. This was to make state-regulated midwives generally available to families that couldn’t afford (n0 health insurance), couldn’t find (due to geographical reasons) or didn’t believe conventional obstetrical care acceptable (due to religious, ethnic traditions, or PTSD).
The legislative intent and provisions of the LMPA and three of its four amendments all materially enhance a midwifery licensing law whose purpose is identified in the “Legislative Intent” as making childbirth safer. The LMPA was to design to achieve these goals by creating a legally-defined mechanism to professionally train and license non-nurse/direct-entry midwives. This was to make state-regulated midwives generally available to families that couldn’t afford (n0 health insurance), couldn’t find (due to geographical reasons) or didn’t believe conventional obstetrical care acceptable (due to religious, ethnic traditions, or PTSD).
All these aspects and implementation serve the intention of the LMPA to make pregnancy and childbirth safer for California families by providing prenatal care, risk screening, referral to medical services as indicated and reducing the risk to mothers and their unborn/newborn babies by eliminating unplanned home births because midwifery care was not available.
Mandatory Obstetrical Consultation and Evaluation under AB 1308
This amendment to the LMPA now requires mandatory obstetrical consultation for possible risk factors, even if this goes directly against the wishes of the childbearing woman and her family. The category of “risks” describes the possibility of a complication in the future but is not itself a present complication that requires any treatment.
The historical and contemporary standard of care as provided by midwives and other maternity care professionals has always required that parents be immediately informed about the presence and nature of any identified risk. When the risk is clinically significant, non-MD practitioners routinely recommend consultation with an appropriate medical specialist. However, parents have a legal right to decline and after carefully pondering the issue, some do. Consultation is not mandatory unless something is really unusual or abnormal and the practitioner believes it would be unethical to continue care without additional information.
Unfortunately, AB 1308 turns all this on its head. It mandates obstetrical evaluation, even when the moter-to-be objects or decline or the health issue involved would more appropriately be referred to another medical specialty (such as an endocrinologist or perinatologist).
Nonetheless, the law stipulates that the pregnant women be seen and evaluated by “a physician with training in obstetrics” before her midwife can provide additional care. Should the childbearing woman be so bold as to exercises her legally-recognized Patients’ Right to refuse any such recommendation, no Californa licensed midwife will legally be able to provide her with additional prenatal care or childbirth services.
If the client agrees to be evaluated by an obstetrician, and can both afford and find an OB in her geographical area who is willing to consult with her, this doctor has a legal duty to the mother under AB 1308 with determining if its appropriate (i.e. in his opinion safe) for the pregnant woman to have a midwife-attend OOH birth in light of the identified risk factor. Of course, this entails enormous legal liability for the obstetrician and so like the issue of obstetricians, the choice that obviously favors the obstetricians is to just refuse to see women referred by midwives.
When obstetricians do evaluate these patients, many routinely recommend against additional midwifery care, thus shielding themselves from all potential legal entanglements. Others OBs agree to examine the woman, but won’t write anything in the medical record, lest they be sued later on. However, without documentable approval by an obstetrician, it’s illegal for the client’s midwife (or any other Ca LM) to provide childbirth services to her.

The consequences of this provision of the LMPA are extremely problematic for all involved (including obstetricians). Under the affects of AB 1308, a significant number of essentially healthy women are needlessly forced into what they believe is an unnecessary (and unwanted) hospitalization and highly-medicalized childbirth under obstetrical protocols.
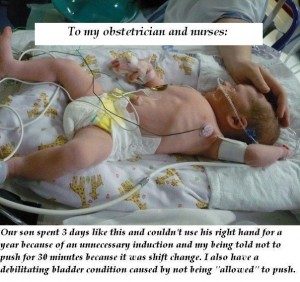 The adjacent photo is from a mother was who was still upset and angry more than a year later about unnecessary intervention in her birth and iatrogenic complications for herself and her baby. She sent this picture of her newborn in the hospital’s NICU to her obstetrician and the L&D nurses, expressing her anger and disappointment.
The adjacent photo is from a mother was who was still upset and angry more than a year later about unnecessary intervention in her birth and iatrogenic complications for herself and her baby. She sent this picture of her newborn in the hospital’s NICU to her obstetrician and the L&D nurses, expressing her anger and disappointment.
The original caption is to small to read, but it says:
“Our son spent 3 days like this and couldn’t use his right hand for a year because of an unnecessary induction and my being told not to push for 30 minutes becasue it was shift change. I also have a debilitating bladder condition caused by not being “allowed” to push.“
In the wake of AB 1308 restriction, a small but still substantial number of these women had such a bad experience with a previous hospital birth that elective hospital birth is out of the question for them. If their local midwives aren’t legally allowed to provide care to them due to restriction introduced by AB 1308, they will look for a lay birth attendant (thus re-inventing unlicensed lay midwifery!) or plan to have an unattended birth.
Up with this we cannot and should not put!
The only appropriate changes to the LMPA are ones that improve access by childbearing families or better meet their needs. while also improving the quality of professional midwifery practice. All future amendments to the LMPA must be sponsored and/or supported by consumer organization such a California Families for Access to Midwifery (C-FAM) and state midwifery organization such as the California Association of Licensed Midwives (CALM) and California College of Midwives (CCM).
All these parameters applied to SB 350 (LMPA) the 1st three amendments (SB 1479, SB 1950, & SB 1638) introduced in 2002, 2002 and 2006. But unfortunately, this was not the case for the amendment introduced in 2013.
AB 1308 directly negated many of the most important the contributions of Licensed Midwifery Practice Act, and the safeguards it provided to childbearing families by making it possible for a trained, experienced and equipped midwife to be present, and in most instances, able to prevent or successfully manage the unexpected problems associated with childbirth, especially as this applies to giving birth in out-of-hospital settings.
This must be fixed and soon.

Midwives and must consumers be (or become) informed about the history of non-nurse midwifery licensing in the State so we can explain it to others and make a compelling case to members of the State legislature.
First, we have to tell our story in order to find an author willing to carry a bill, and then we have to convince a sufficient number of legislators to support our efforts. This is especially critical for the seven Legislators who sit on the Business and Professions Committees of both chambers, a who can so easily kill a bill long before a floor vote.
To better understand the reasons why AB 1308 is not just bad policy for Ca LMs, but also unconstitutional from the perspective of childbearing families, please continue reading:
Associated Topic –> The Obstetrical Standard of Care in the US – Historically Illogical, Fundamentally & Fatally-flawed
Reference #1:
Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31:
This control group consists of women with the same general health and demographic characteristics that are seen in the CDC birth registration data. This is predominately healthy, white, middle-class women who had economic access to all categories of maternity care providers and settings, but in this case, purposefully choose unattended births.
Data on this group of unattended home births came from Indiana state mortality statistics for a fundamentalist religious group that rejected all forms of medical care under all circumstances – no prior diagnosis or treatment of chronic medical problems, no risk-screening of mothers during pregnancy, no prenatal care, no trained attendant during childbirth and no emergency transfer of mother or baby with life-threatening complications to a medical facility – a situation similar to rural parts of the developing world.
Out of 344 births, the unattended group had 6 maternal deaths and 21 perinatal losses. The baseline mortality rate for unattended childbirth was one maternal death per 57 mothers or MMR of 872 per 100,000 live births (92 times higher than Indiana’s MMR for the same period) and one perinatal loss for every 16 births or PNM rate of approximately 45 per 1,000.