Scroll to bottom to watch the last half of the Feb 3rd MBC’s Quarterly meeting ~ physicians discussing the proposed Mfry regulations.
Continuation of information about proposed mfry regulations:
Proposed Reg #2 – Access to necessary medical supplies, prophylactic & emergent drugs
The 1993 LMPA modernized the traditional practice of midwifery by incorporating midwifery training that was ‘equivalent but not identical’ to California requirements for nurse-midwives and authorizing the use of a limited number of specified drugs and medical supplies that are for preventive and/or emergent use. This is qualitatively the same as the authorizing legislation of many other non-physician practitioners already referred to in parts one and two of this communication.
* Rhogam for Rh-negative women to prevent fetal death or mental retardation from erythroblastosis fetalis in subsequent pregnancies
* antibiotic ophthalmic ointment for newborns as required by state law to prevent blindness from ophthalmia neonatorum
* vitamin K to prevent death or permanent neurological injury resulting from the hemorrhagic diseases of the newborn.
The LMPA also provides for didactic education as well as clinical training in the emergent use of drugs and medical supplies. In addition to 36 hours of CEUs necessary for bi-annual license renewal, LMs must also be re-certified in adult & infant CPR and neonatal resuscitation every 2 year. LMs take the same national neonatal resuscitation course required for hospital NICU personnel. As an interesting aside, obstetricians no longer provide care to neonate at delivery, so while midwives have to be certified in neonatal resuscitation, obstetricians don’t have to be.
Emergent drugs and materials includes:
* oxygen (emergency response to respiratory distress in mother, fetus, or neonate)
* lactated ringer’s IV solutions (severe dehydration or excessive bleeding)
* post-partum use of oxytocins (Pitocin, Methergine, etc) to stop excessive maternal bleeding or stabilize a postpartum hemorrhage while awaiting hospital transport
* injectable local anesthetic and other materials for suturing perineal lacerations
With the exception of oxygen, all the specific drugs noted above were not yet invented in 1917, when the original statutory scheme for traditional midwifery was created. Access to and use of these drugs and medical supplies was specific to modernizing the traditional practice of midwifery in California in 1993. This was based on the established ability of these medical products and pharmaceutical agents to improved patient safety by preventing disease states and providing an effective emergent response to complications that reduce the risk that relatively minor problems will turn into preventable life-threatening emergencies.
While many of these life-saving substances are ‘medicines’ in the sense of pharmaceutical agents, they are not per se the private property of the medical profession. The authority of the medical profession is derived solely from the State Legislature, which reflects the will of the citizens of California to promote public safety through out the health and emergency medical care system. I think most Board members will agree that a huge amount of public and charitable funds (state, federal and private) for higher education and research into many overlapping medical and healthcare fields (including cognitive science and computer technologies) goes to the betterment of the human condition. Ultimately these advances belong to all of humanity, which include making life-saving drugs and medical supplies ‘appropriately’ available to residents of California.
For example, a Quaker wildness camp for teenagers high in the Trinity Alps provides all of its camp counselors with ‘epi’ pens in case one of the kids has an anaphylactic reaction to a bee sting. These counselors do not have ‘physician supervision’ and yet they are not considered to be practicing medicine without a license.
Drugs/techniques in the LMPA that are NOT taught or used by LMs.
While ‘analgesics’ are mentioned in the authorized drugs listed in the LMPA as part of mfry training and practice, no pain medication (either OTC or Rx) are ever administered by LMs in an OOH setting. Period. I carry NO pain-relieving drugs in my little black bag (only ibprophen in my pocket in case i get a headache).
If the non-drug methods of pain relief typically used by midwives don’t work and the mother can’t tolerate an unmedicated labor (or doesn’t progress as expected), then we transfer her to a nearest appropriate hospital. As documented in the LMAR for 2007 through 2011, ‘request for pain medication’ is the single most frequent reason for hospital transfer of laboring clients.
When we arrive at the hospital, a qualified anesthesiologist is contacted and generally delighted to provide epidural analgesia, while both mother and midwife are equally happy that such an effective and safe method of pain control is available. Midwives don’t see this as a ‘failed home birth’ but an appropriate hospital transfer. This means the midwife is doing her professional job, which includes facilitating timely access to necessary medical interventions. As I mentioned at the Feb 3rd Board meeting, midwives and obstetricians are (or are suppose to be) on the same team, working for the same goal – good maternal-infant outcomes, which includes HAPPY moms. I’ve never seen a new mother be happy unless her baby was also healthy.
Para-cervical and pudental blocks are also listed in the LMPA, but use of these techniques are NEVER taught to mfry students, and NEVER used by Cal. licensed midwives. Inclusion of these techniques in our licensing law was a statutory fluke. The author in the LMPA wanted to avoid the public confusion and practitioner inequality and potential discrimination that would come from legislating two different levels or types of midwifery in California. Inevitably one would be considered better and the ‘lesser’ category would be denigrated, thus creating all kinds of mischief.
So Senator Killea copied the wording for the LMPA in toto from the 1974 nurse-midwifery act — same educational curriculum, same scope of practice, even the same misspelling of the word ‘episiotomy’. Since CNMs primarily practice in hospital setting, these anesthetic techniques were appropriately part of the 1974 nurse-midwifery law, but are never appropriate in any OOH setting, irrespective of LM vs CNM licensure.
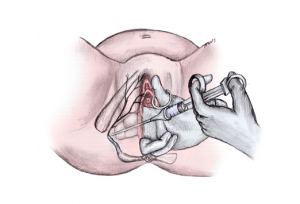 As you already know, neither obstetrical anesthetic technique is a part of the contemporary standard care for either physicians or midwives. In particular, para-cervical blocks can be extremely dangerous, as injecting a large bolus of Lidocaine (10 cc’s) or similar local anesthetic into the mother’s para-cervical tissue in the few minutes just prior to birth inadvertently exposes the fetus, via transfer from the mother’s blood stream, to an adult dose of this potent drug. This is associated with a profound cardiac and respiratory depression in the newborn (gray baby syndrome).
As you already know, neither obstetrical anesthetic technique is a part of the contemporary standard care for either physicians or midwives. In particular, para-cervical blocks can be extremely dangerous, as injecting a large bolus of Lidocaine (10 cc’s) or similar local anesthetic into the mother’s para-cervical tissue in the few minutes just prior to birth inadvertently exposes the fetus, via transfer from the mother’s blood stream, to an adult dose of this potent drug. This is associated with a profound cardiac and respiratory depression in the newborn (gray baby syndrome).
Para-cervical and pudental blocks are not and will not ever be used by LMs or CNMs. Since passage of these laws in 1974 and 1993, both out-dated anesthetic techniques have been replaced by a much better and safer choice — your favorite and mine — epidural analgesia.
Future Communications
Many other topics vital to the regulatory issues of licensed midwifery were not addressed in this communication.
As I mention when we spoke in person after the Feb. 3rd meeting, an informational 3-ring notebook for new members of the Midwifery Council, agency staff and Board members is available in both hard copy and on-line versions. It provides pertinent background material on the history of traditional (non-medical, non-nurse) midwifery in California and contemporary information on the educational requirements and our scope of practice.
If you will provide me with an office address or PO Box# via return email, I will send you a copy.
warmest regards ^O^
Faith Gibson, LM, CPM, former Chair, MBC’s Midwifery Advisory Council (2007-2010)
Re-appointed in 2010, current Member of the Midwifery Council
[youtube]http://www.youtube.com/watch?v=X7_aUMKMobc&feature=plcp[/youtube]
1 comment
Comments are closed.